The latest EHV/EHM outbreak has confirmed 50 total positive horses: 34 linked to the Waco, TX WPRA event and 11 not associated. With 28 neurological EHM cases and 152+ exposed horses across multiple states, learn key biosecurity measures and how to protect your horses from this highly contagious virus.
This data was compiled at 9:30 am Central Time on 11/26/2025 from EDCC's published information. Updated 12:35 PM Central Time
This report provides a summary of the Equine Herpesvirus (EHV) and Equine Herpes Myeloencephalopathy (EHM) cases reported from October 20, 2025 up to November 25, 2025. The data is categorized based on association with the Women's Professional Rodeo Association (WPRA) event in Waco, Texas.
Table of contents [Show]
Overall Findings
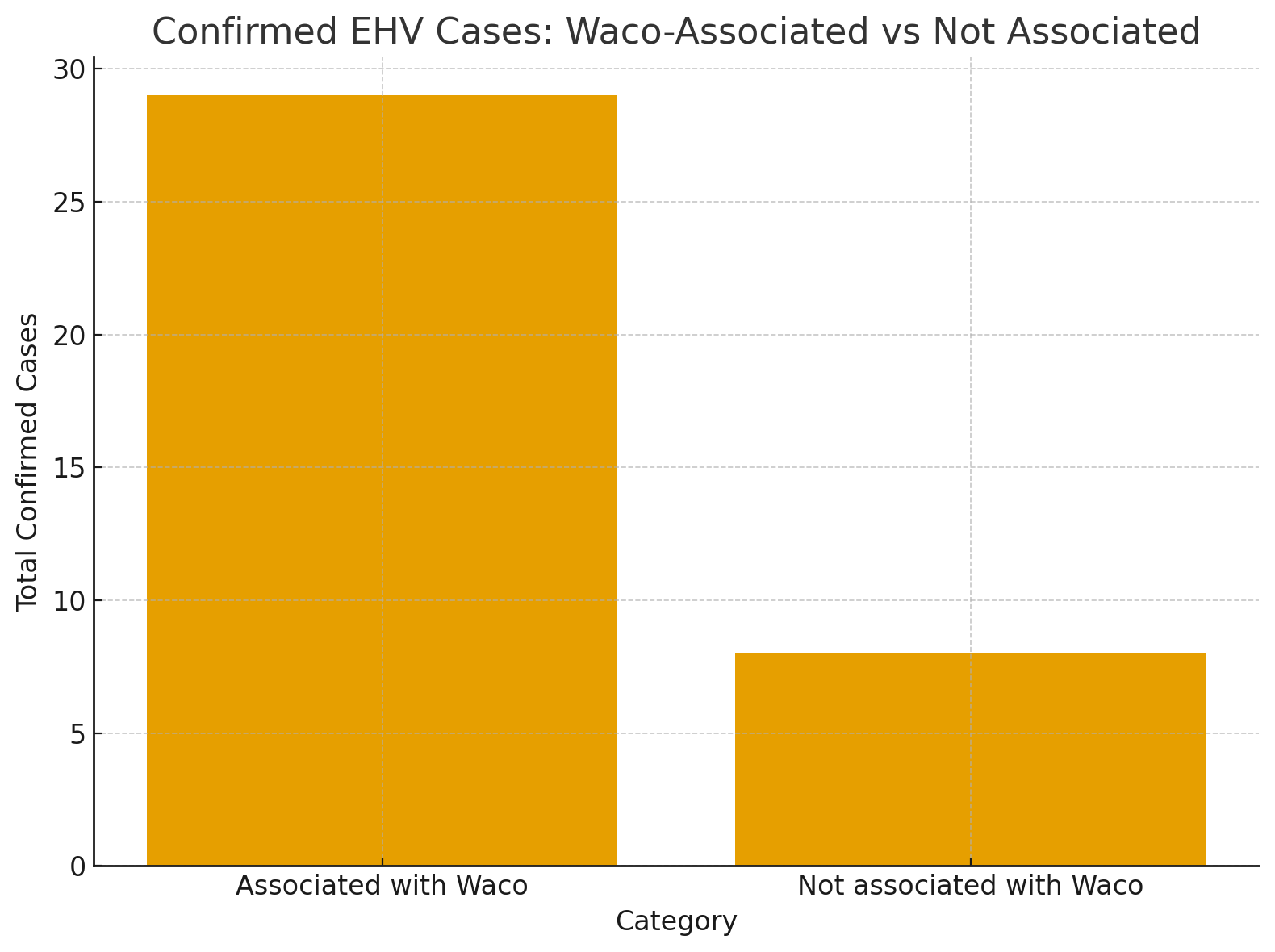
Across all reported locations, a total of 45 horses have been confirmed positive for EHV/EHM. These cases have led to the exposure of at least 152 additional horses. Tragically, 5 of the confirmed positive horses have been euthanized.
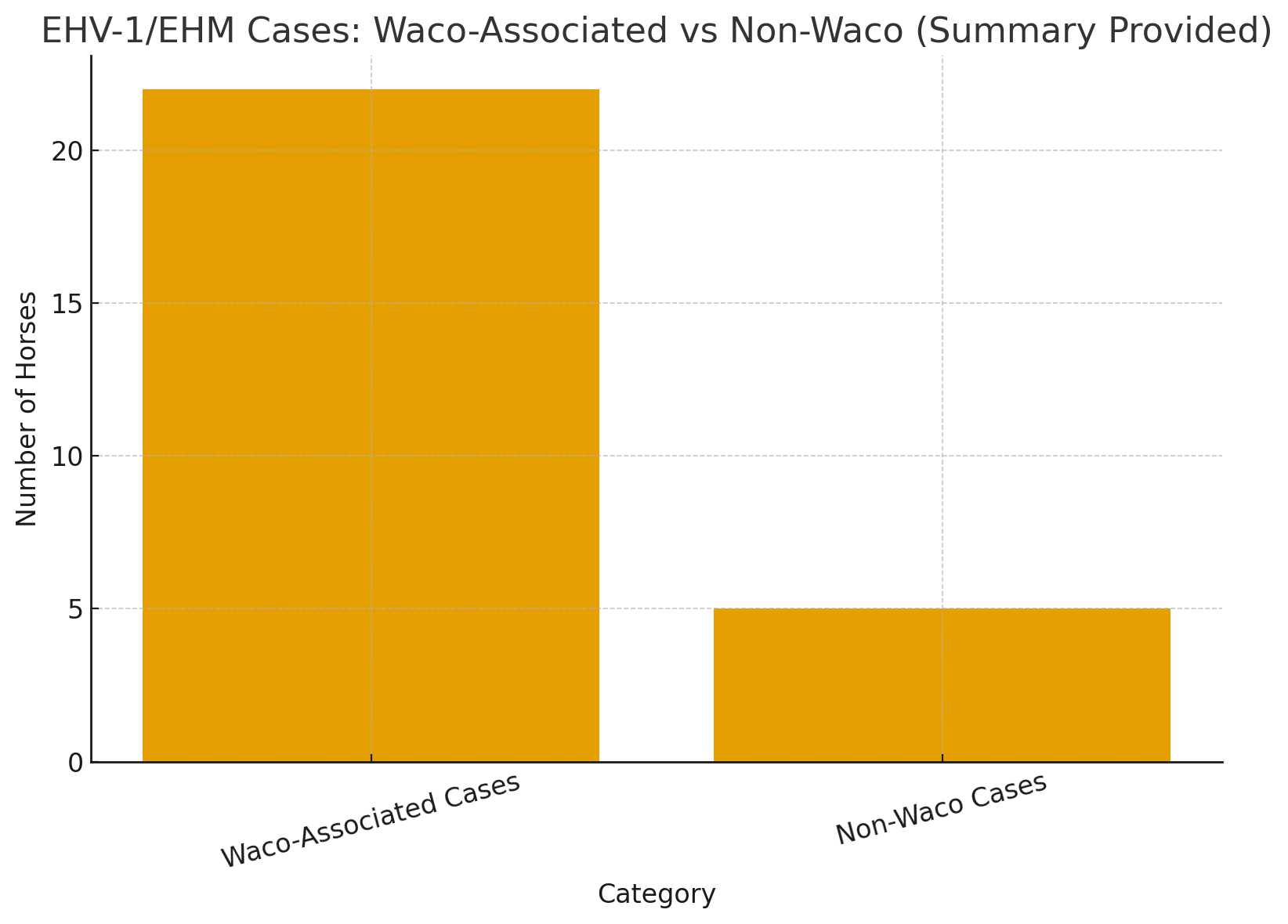
Of the confirmed cases, 28 horses presented with neurological symptoms (EHM), representing a significant portion of the severe outcomes.
Waco Event Outbreak Analysis
The outbreak originating from the Waco, TX event is the primary driver of the current cases.
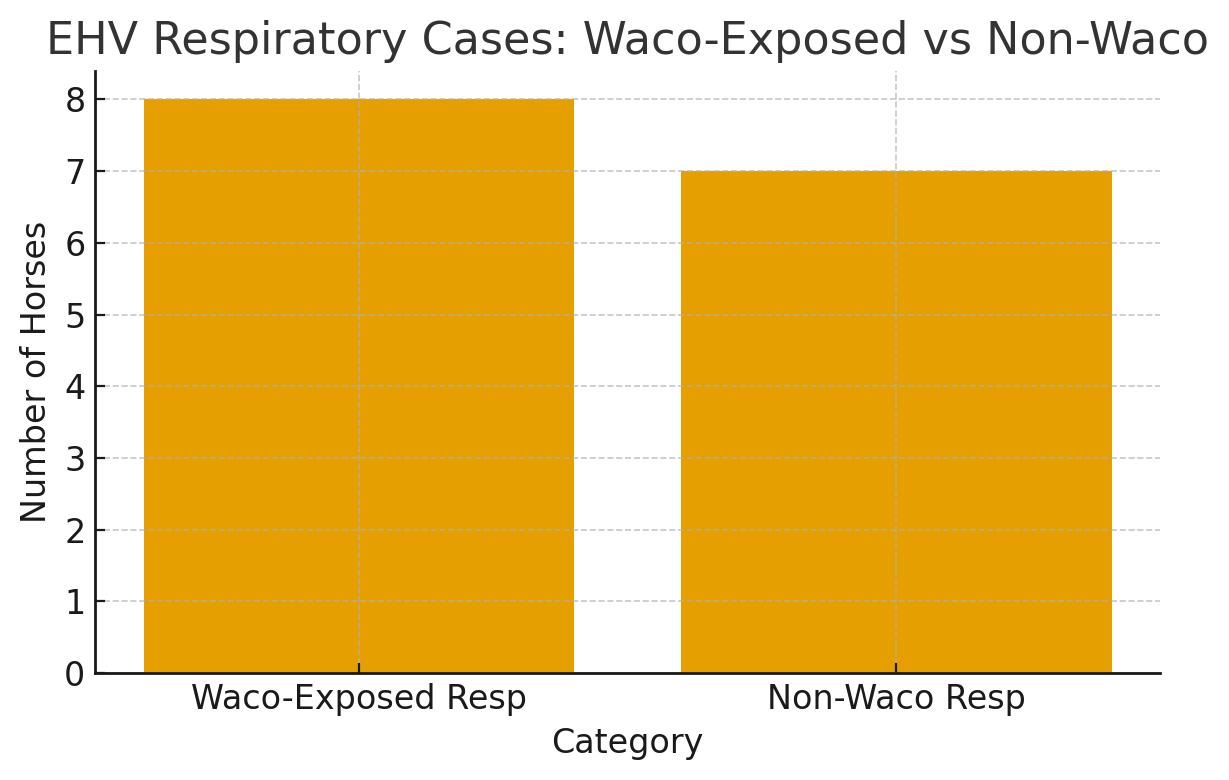
- Confirmed Cases: A total of 34 confirmed positive horses are directly associated with the Waco event. This accounts for 78% of all reported cases.
- Neurological Impact: Of the Waco-associated cases, 27 horses developed severe neurological symptoms (EHM).
- Exposed Horses: Within this group, 55 horses have been officially reported as exposed to a direct positive case. (exposed following event)
- Fatalities: 3 of the total euthanasias are linked to horses that attended or were exposed through the Waco event.
The geographic spread from this single event is extensive, with positive cases identified in Texas, Oklahoma, Arizona, Washington, Colorado, South Dakota, New Mexico, and Louisiana.
Counties where those horses are located
Texas
- Montgomery County: 2 EHM cases (1 euthanized), 1 EHV case (no clinical signs).
- McLennan County: 2 EHM cases (1 hospitalized).
- Wharton County: 1 EHM case, 9 exposed horses.
- Bell County: 1 EHM case (euthanized).
- Fort Bend County: 1 EHM case, 2 exposed horses.
- Erath County: 2 EHM cases.
- Wise County: 1 EHM case, 1 suspected positive.
- Hood County: 1 EHM case.
- Parker County: 1 EHM case (euthanized).
- Randall County: 1 EHM case.
- Lee County: 1 EHM case.
Oklahoma
- Logan County: 2 EHM cases.
- Mayes County: 1 EHM case.
- Oklahoma County: 1 EHV case (no neurological signs).
- Love County: 1 EHM case (mild neurological signs).
Louisiana
- East Baton Rouge Parish: 3 EHM cases (treated at LSU Veterinary Hospital).
Colorado
- Larimer County: 1 EHM case.
New Mexico
- Dona Ana County: 1 EHM case, 2 exposed horses.
- Eddy County: 2 EHM cases, 3 exposed horses.
Washington
- Spokane County: 2 EHV cases (mild fevers, no neurological signs).
Arizona
- Maricopa County: 3 EHV cases (no clinical signs), 5 exposed horses.
South Dakota
- Hyde County: 1 EHM case, 1 exposed horse.
Non-Waco Associated Cases
A smaller number of cases have been reported that are not linked to the Waco event.
- Confirmed Cases: There are 11 confirmed positive horses in this category.
- Neurological Impact: 1 of these horses presented with neurological symptoms.
- Exposed Horses: This group accounts for 97 exposed horses, largely driven by a single outbreak at a private facility.
- Fatalities: 2 euthanasias were reported from cases not associated with the Waco outbreak.
These unrelated cases were identified in Ohio, Pennsylvania, Montana, Wisconsin, Maryland, and two Canadian provinces (Alberta and Ontario), indicating separate and distinct instances of EHV activity.
Counties/ Regions where those horses are located
Ohio
- Madison County: 1 EHV case.
Pennsylvania
- Northumberland County: 1 EHV case.
Montana
- Beaverhead County: 5 EHV cases.
Wisconsin
- Waupaca County: 1 EHV case.
Maryland
- St. Mary’s County: 1 EHM case (euthanized).
Canada
- Alberta (AB): Red Deer County: 1 EHM case.
- Ontario (ON): Regional Municipality of Waterloo: 1 EHM case.
Key Insights
The data clearly indicates that the WPRA event in Waco, TX, has been a mass-spreader event, responsible for the vast majority of current EHV/EHM cases and the wide geographic distribution of the outbreak. While other unrelated cases exist, the scale of the Waco outbreak with EHM cases highlights the critical importance of biosecurity protocols at large equine gatherings. The number of horses presenting with severe neurological forms of the disease is a significant concern for animal welfare.
Vaccines
Current EHV vaccines are primarily designed to help prevent the respiratory and abortion-causing forms of EHV-1. While vaccination can reduce the severity of disease and help control the spread of the virus, it is important to note that no vaccine offers full protection against the neurological form of the disease, known as equine herpesvirus myeloencephalopathy (EHM). Despite vaccination efforts, neurological EHV outbreaks continue to occur. For more detailed information, horse owners are encouraged to review guidelines and research from trusted sources such as the American Association of Equine Practitioners (AAEP), and consult with their personal veterinarians.
FAQ:
Q: What is equine herpesvirus (EHV)?
A: Equine herpesvirus (EHV) is a highly contagious virus that affects horses and can cause respiratory disease, abortion in pregnant mares, neonatal death, and a severe neurological form known as equine herpesvirus myeloencephalopathy (EHM). There are several strains, but EHV-1 and EHV-4 are the most common and clinically significant.
Q: How is EHV transmitted between horses?
A: EHV is primarily spread through direct horse-to-horse contact, but it can also be transmitted indirectly via contaminated equipment, clothing, human hands, and airborne particles over short distances. The virus can survive on surfaces for a period, making biosecurity measures crucial.
Q: What are the symptoms of EHV?
A: Symptoms can vary based on the type of EHV but commonly include fever, nasal discharge, coughing, lethargy, loss of appetite, and swollen lymph nodes. Neurological symptoms of EHM include incoordination, hind limb weakness, inability to stand, and in severe cases, paralysis.
Q: Is there a treatment for EHV?
A: There is no specific antiviral treatment for EHV. Supportive care such as anti-inflammatory medications, fluids, and rest is typically provided to affected horses. Isolating infected individuals is key to preventing the spread of the virus.
Q: How effective are EHV vaccines in preventing the disease?
A: While EHV vaccines can reduce the severity of respiratory symptoms and the risk of abortion in pregnant mares, they are not fully effective in preventing neurological EHM. Even vaccinated horses can contract and spread the virus under certain conditions.
Q: What biosecurity measures help prevent EHV outbreaks?
A: Good biosecurity practices include isolating new or returning horses for at least 21 days, avoiding shared equipment, regular cleaning and disinfecting of stables and tools, minimizing horse-to-horse contact at events, and practicing proper hygiene after handling horses.
Q: What should I do if an EHV outbreak occurs at my facility?
A: If an outbreak is suspected, immediately isolate affected horses, contact your veterinarian for guidance, and implement strict biosecurity protocols to prevent further spread. Notify others who may have been in contact with your horses and comply with local regulations regarding disease containment.
Q: Where can I find more information on EHV?
A: Reliable information on EHV can be found through trusted organizations such as the American Association of Equine Practitioners (AAEP), university extension programs, and your local or state veterinary services. Consulting with your veterinarian is also highly recommended for tailored advice.
Q: What are the recommended biosecurity measures to prevent the spread of EHV?
A: Implementing strong biosecurity practices is crucial in preventing the spread of EHV. The following measures are recommended:
- Isolate new or returning horses: Quarantine new arrivals or horses returning from events for at least 21 days to monitor for any signs of illness.
- Minimize horse-to-horse contact: Avoid unnecessary contact between horses, especially among those from different barns or locations.
- Use individual equipment: Each horse should have its own halter, lead rope, grooming tools, and feed/water buckets to prevent cross-contamination.
- Maintain cleanliness: Regularly disinfect shared surfaces such as stalls, fences, trailers, and wash racks using an effective equine-safe disinfectant.
- Practice good hygiene: Wash hands thoroughly with soap and water between handling different horses, and wear protective clothing when dealing with sick animals.
- Monitor health closely: Regularly check all horses for signs of illness and immediately isolate any horse showing symptoms of infection.
- Limit access to the barn: Restrict visitors and ensure anyone entering your facility adheres to established biosecurity protocols.
- Vaccinate appropriately: Consult with your veterinarian to develop a vaccination schedule tailored to your horse's specific needs and risk factors.
- Transport safely: Clean and disinfect trailers before and after every use, and minimize sharing of transportation equipment with other horse owners.
- Keep detailed records: Maintain records of all horse movements, health statuses, and vaccination histories to track potential exposures.
Following these biosecurity measures can help reduce the risk of EHV transmission and protect the overall health of the equine community.